Ushering in genetic evaluation for Usher Syndrome
Sep 18, 2017
22431 Views
This could be the first time you’ve heard about Usher syndrome. That’s ok. You may not know what kind of a condition it is. That’s ok, too. But, by the end of this post, you will have an understanding of what it is, its symptoms, when to seek genetic expertise, and what can be done in order to manage Usher syndrome. You know what else? You may even be able to explain what a genetic syndrome is to your friends and colleagues. Now that, is awesome! So let’s get started right away!
A syndrome is a disease or disorder that has more than one feature or symptom. Usher syndrome is a genetic condition that can be caused by mutations in several different genes. We’ll discuss what those are in detail; just a little while later.
First, Usher syndrome is characterized by the following 2 main features (or symptoms):
- Hearing loss
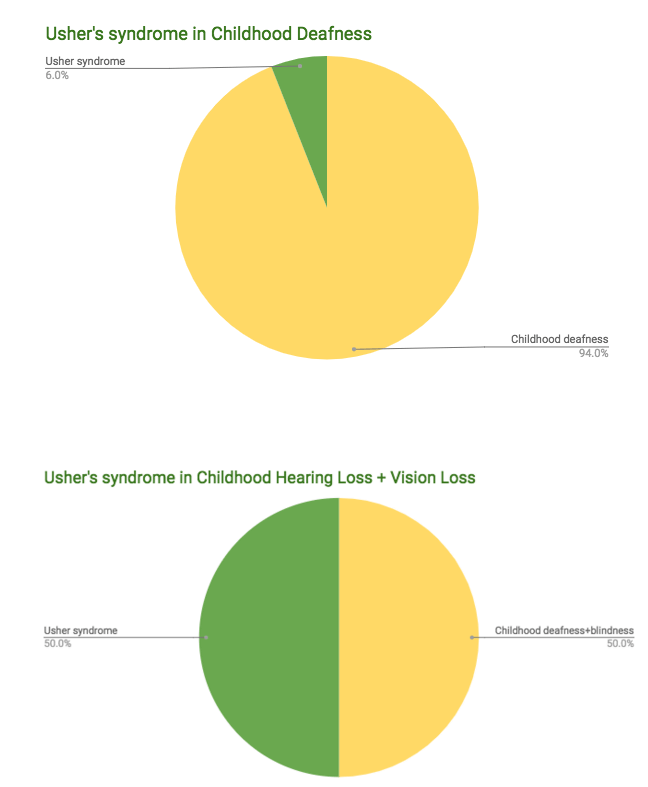
An individual with Usher syndrome is often times first brought to medical attention because of either partial or total hearing loss. The type of hearing loss associated with Usher syndrome is classified as sensorineural hearing loss (SNHL), which means that it is caused by abnormalities of the inner ear. Accounting for about 90% of reported hearing loss, SNHL is extremely common type of hearing loss. And amongst various kinds of SNHL, Usher syndrome is one of the most common syndromic forms of hearing impairment. In fact, while Usher syndrome is seen in only up to 6% of children with hearing loss, when vision loss is added to the evaluation criteria (syndrome = one feature + another feature, remember?), Usher syndrome is the most common genetic condition affecting both hearing and vision. It is prevalent in 50% of all deaf-blindness.
- Vision loss
The loss of vision in Usher’s is caused by an eye disease called retinitis pigmentosa (RP), which affects the layer of light-sensitive tissue at the back of the eye (the retina). As the light-sensing cells (rods) of the retina gradually deteriorate, vision loss occurs. Typically, night vision is the first to get affected, and it is followed by the development of blind spots in peripheral (side) vision. Over time, these blind spots enlarge and merge, causing loss of peripheral vision with the retention of central vision. This is known as tunnel vision, which is often described as “seeing through a straw”. In some cases, vision is further impaired by clouding of the lens of the eye (cataracts). However, many people with retinitis pigmentosa retain some central vision throughout their lives.

There are 3 major types of Usher syndrome identified– types I, II and III (no points for creativity or guesses there!). These are largely distinguished by the severity of hearing loss, the presence or absence of balance problems, and the age at which signs and symptoms appear.
| Usher Syndrome | Type I | Type II | Type III |
| Hearing | Profound deafness in both ears at birth | Moderate to severe hearing loss at birth | Normal at birth; progressive loss in childhood or early teens |
| Vision | Decreased night vision before age 10 | Decreased night vision begins in late childhood or teens | Varies in severity; night vision problems often begin in teens |
| Vestibular function (balance) | Balance problems at birth | Normal | Normal to near-normal, chance of later problems |
Type I
- The hearing loss in Usher syndrome type I is congenital (present at birth), bilateral (affecting both ears), and profound (severe). As a result of this profoud hearing loss, affected individuals do not develop speech.
- A defining feature of this condition is ‘vestibular areflexia’, an abnormality in the part of the inner ear that helps maintain the body’s balance and orientation in space. As a result, children with the condition have trouble with balance. They begin sitting independently and walking later than usual at approximately (at age 18 months to two years), they may seem ‘clumsy’ or have frequent accidental injuries, or have difficulty with activities that require balance (such as riding a bicycle and playing certain sports).
- The child with Usher syndrome type I is often misdiagnosed as having nonsyndromic deafness until tunnel vision and night blindness, early signs of retinitis pigmentosa (RP) become severe enough to be noticeable, either by parents at home, teachers at school, or by the individual themselves.
Type II
- The hearing loss in Usher syndrome type II is also congenital, bilateral sensorineural hearing loss. However, the severity is considered is mild to moderate for low frequencies and severe to profound for higher frequencies. For example, it is difficult for affected individuals to hear high, soft speech sounds, such as those of the letters ‘d’ and ‘t’. Needless to say audiology evaluations are critical in establishing the type of hearing loss and facilitating accurate diagnosis.
- One of the most important clinical distinctions between Usher syndromes type I and II is that children with Usher syndrome type I are usually delayed in walking until age 18 months to two years because of vestibular involvement, whereas children with Usher syndrome type II usually begin walking at approximately age one year. Vestibular responses in individuals with Usher syndrome type II remain intact, and individuals typically have no issues related to walking, running or balance
- Retinitis pigmentosa (RP) is of adolescent-to-adult onset
Type III
- People with Usher syndrome type III experience hearing loss and vision loss beginning somewhat later in life. Unlike the other forms of Usher syndrome, type III is usually associated with normal hearing at birth. Hearing loss typically begins during late childhood or adolescence, after the development of speech, and becomes more severe over time. By middle age, most affected individuals have profound hearing loss.
- Vestibular responses Some people with Usher syndrome type III develop vestibular abnormalities that cause problems with balance
- Vision loss caused by retinitis pigmentosa also develops in late childhood or adolescence. Some people with Usher syndrome type III develop vestibular abnormalities that cause problems with balance.
Usher syndrome has genetic heterogeneity, which means that it can be caused by mutations in one of several different genes. Mutations in at least six genes can cause Usher syndrome type I. The most common of these are MYO7A gene mutations, followed by mutations in the CDH23 gene. Usher syndrome type II can result from mutations in three genes; USH2A gene mutations account for most cases of type II. Usher syndrome type III is most often caused by mutations in the CLRN1 gene.
| Usher syndrome | Genes involved |
| Type I | MYO7A, CDH23, USH1C, PCDH15, USH1G, CIB2 |
| Type II | USH2A, ADGRV1, WHRN (DFNB31) |
| Type III | CLRN1, HARS |
All of the types of Usher syndrome are inherited in an autosomal recessive pattern, which means both copies of a gene in each cell have a mutation. The parents of an individual with Usher syndrome each carry one copy of the mutated gene, but they do not have any signs and symptoms of the condition. For this reason, most families discover their carrier status of Usher syndrome only after the birth of an affected child. Carrier parents of autosomal recessive conditions have a 25% chance – every pregnancy- of having a child with that condition. Genetic testing can help identify the gene responsible for a child’s Usher syndrome and confirm the carrier status of parents. Such genetic counseling and testing achieves important healthcare goals:
- It can guide appropriate clinical management of the child in terms of surveillance for and treatment/management of presenting symptoms
- Additionally, it plays a critical role in anticipating other known symptoms of Usher syndrome (such as cataracts). This facilitates the development and execution of a long-term plan for necessary health care and management.
- Further, it facilitates the identification of genes/mutations specific to the family and can inform recurrence risks and reproductive decision making
- Finally, it empowers families to cope with and successfully adapt to the medical, familial, and psychological ramifications of a genetic condition
Now that you’re ready to be a responsible and educated participant in your family’s health care, it’s time to spread the word about Usher syndrome. Hearing loss is extremely common. Couple that with vision loss, and you’ve a high chance that you’re looking at Usher syndrome. Genetic syndromes may seem intimidating to understand, diagnose and manage. Luckily, genetic counselors are health care practitioners with expertise in medical genetics and psychological counseling to help you learn about how your DNA impacts you and your family. Setting up a genetic counseling appointment can help every individual learn about what their medical and family history may mean for themselves, and can set them up on the right path to medical care, health, and wellbeing.
If you or your child has hearing loss and you would like a genetic evaluation, speak with a genetic counselor.


