The Immune system warriors: GAMED antibodies
Mar 29, 2020
37469 Views
Anu Acharya, CEO Mapmygenome
Under the fortress of our skin
and in the bloodstream
I saw some antibodies go by.
In the case of a Covid attack
They decide to quickly multiply
Primarily leading the battle with G &M
When it comes to law and order, the police is what comes to mind. When things go out of control, sometimes we need to bring in the army. Sadly, we also saw that Covid has caused enough challenges to bring in the army in cities like London, with the hope that the lockdown can flatten the curve for the virus and our ecosystem is better equipped with tests, medicines, protective gear, and ventilators.
Two kinds of Immunity- Innate and Adaptive
Our immune system is in many ways like the defenSe system for our body.
One part is innate and the other is adaptive, rising to the occasion when invaders attack our body, the pathogens.
The surface of all cells has some form of a special marker called an ‘antigen’, which is a protein that tells the immune system to respond. The immune has to determine if the invader is either “self”, “non-self” or an “allergen”. “Self” implying part of the system, so no immune response is created, a “non-self” or foreign particle will trigger an immune response, and an “allergen” creates overreaction. In the case of COVID, it would be a non-self particle/pathogen that initiates an immune response. The immune system is a complex system with several different elements. I will only discuss a few relevant ones for now.
T cells and B cells
The main cells of the immune system are White Blood Cells known as B cells and T cells. B cells are produced and mature in Bone marrow but can also be found in lymph nodes. T cells are also produced in bone marrow, but they mature in the Thymus and thus T cells. There are three types of T cells: a helper T cell, a Killer T cell, and a memory T cell that remembers the invaders.
Innate immunity
When a pathogen like a virus or bacteria invades, our “inner army” has several lines of defenses to deal with the invaders:
- The first defense is our skin, which is like the walls built around the city to physically protect us.
- The second layer of defense are non-specific antibodies, that we already have in store, that attack the pathogens and cause inflammation and fever. Inflammation comes up when the pathogen signals the blood cells to increase its numbers around the infected area. Then the white blood cells or WBCs create those little monsters called phagocytes that engulf the pathogens like in a video game. If you wondered why you get a fever, it is because your body’s defence system knows that high body temperatures don’t allow pathogens to survive.
Adaptive Immunity
The Adaptive Immune system is a secondary immune response to a highly specific pathogen. Dendritic cells are the main cells that connect the adaptive immune system to the innate immune system Dendritic cells are an interesting shaped accessory that helps bond the immune systems together like the slogan of the brand “Dendrite Gum”.
These dendritic cells first eat up a few of the invaders and then rush using the lymph glands to a lymph node where they quickly report the exact location of the attack to the T-cells. This is how highly specialized and adaptive immunity comes to the playground of invaders. Think of the accessory cells (aka dendritic cells) as Narad Muni passing on messages between our innate and adaptive immune systems. The only difference is that he has himself eaten some of the enemies to tell which kinds of cells to attack instead of reciting poetry or telling stories.
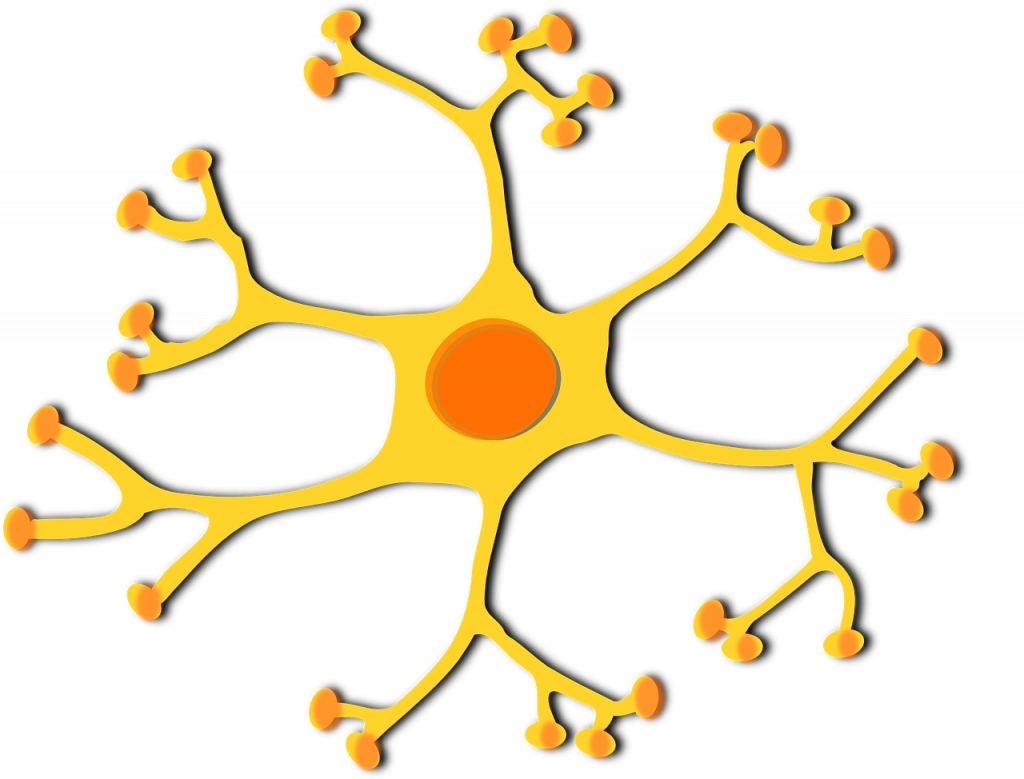
These dendritic cells that have just engulfed our virus (the invader) attach to some specific type of T-cells. These T-cells start to multiply and prepare to attack this specific invader. Other helper T-cells help the rest of the immune system get into action. If the same invader comes once again, phagocytes (our video game monster) can do what our dendritic cells did when the invader came in for the first time. Memory T-cells help remember the previous attack.
Once this immune system has attacked invader cells, they get marked as safe, so that only the invaders can be specifically targeted. Our defence system also has a way of remembering the pathogens that invaded so that they can respond to them quickly by referring to a curated rap-sheet of past invaders.
Role of genes?
As humans, we are all 99.9% alike but 0.1 % different. The biggest difference is in the genes that code for the immune system and our dendritic cells that have different structures for people with different genetic codes. This difference can play a key role in explaining why some of us respond well to infection while others don’t.
Genes regulate immune processes by controlling antibody production, function, and signalling. Dysregulation of the immune response (e.g., autoimmune disease) also has a significant genetic contribution from genes of the interleukin family (ILs), human leukocyte antigen family (HLA), and many more.
Also Read:
GAMED how?
Antibodies are Y-shaped molecules comprising 4 chains — 2 are heavy and 2 light chains — joined by sulphur bonds. While most antibodies are of a simple Y-shape, some of these antibodies form intricate and beautiful structures like a pentamer (5 units) or dimer (2 units) that look like snowflakes.
There are 6 types of heavy-chains — the Gamma, Alpha, Mu, Epsilon, and Delta — an easy way to remember them is with the word is GAMED; the light-chains are 2 in number and can be either Kappa or Lambda, and that marks the end of today’s lesson in greek alphabets. For COVID, two antibodies are the most important: IgG and IgM.
IgG
IgG, the most common antibody, is found in the plasma cells. They are produced during both the primary and secondary immune response, bind to the antigen (or virus), and prevent it from infecting more healthy cells. Its structure is a monomer (a single, Y-shaped antibody). These antibodies, on account of their monomeric structure, are small enough to be transferred across the placenta. In fact, all of us got our first antibodies from our mother, in-utero, for “passive” immunity. As we grow older, IgGs originate from our lymph nodes. These antibodies have the longest half-life amongst all the antibodies — 23 days, to be precise — and confer long-term immunity. When we are looking at infection levels, these IgGs would show up in the blood even after recovery and indicate a history of an old infection among currently healthy people.
IgM
IgM is the first antibody that is produced in response to an infection or a pathogen attack. Being a pentamer, it is fairly large in size, and thus cannot be passed from mother to child. This is a rather efficient antibody against infection, and the identification of IgM in the blood often indicates a new infection.
The other 3 antibodies
A little about the other three even though it may not be relevant for now.
- IgE is present in small quantities and is found more when we have an allergic reaction
- IgA is found in secretions like our sweat
- IgD is supposed to be a B-cell receptor
The making of the antibodies from B-cells with a little help from T-cells.
Think of B-cells as a place where they receive the antigen (e.g., from coronavirus). It breaks it down and creates an MHC2, a complex-sounding term with the word complex in it. It is called the major histocompatibility complex 2. The MHC2 allows the helper T-cells to bind to it and they release lymphokines (signalling molecules) that multiply, become plasma cells, and release antibodies that are specific to the antigen (from our coronavirus in question). This is where the antibodies come from. If this was confusing, allow me to simplify: the B-cells, with some help from helper T-cells, produce specific antibodies. Clear?
The killer T-cells recognize infected cells with the markers on them and start killing them by a process known as apoptosis or programmed cell death. I remember that term from high school.
How does an antibody test work for Covid?
Almost everyone I know is intrigued by COVID testing. Other than a confirmatory test done by RT-PCR that I have covered in past blogs, one of the ways to assess the spread of the disease and quickly look at a pandemic spread in a population is to use Rapid diagnostics that require neither a lab nor trained professionals, and can be easily done from the convenience of one’s home. A good example of such a rapid diagnostic test is the home pregnancy test. There are also tests that can be done in a laboratory; these tests fall under what we call ‘serological tests’.
Serological Tests
A serological test, as the name suggests, is the study of our blood serum. Now you may wonder what serum is? It is the clear liquid (yes, clear) that separates from the blood when it is allowed to clot. We can then look for the antibodies in our blood.
Rapid Diagnostics
Rapid Diagnostics tests as quickly discussed earlier, are like pregnancy tests. They can identify if we have ever been infected with COVID. Further, there are many more technologies that are available to detect antibodies, and I will write more on each in the next blog.
The antibody warriors that circulate in our blood help us understand our defense system better. We can help build a better defense system when we eat better, exercise and sleep, and with a little help from our genes.
The Covid Blog Series –
1. The Pandemic of our times
2. 10 ways to defend yourself from Covid
3. The Science behind Covid for the Avid Reader
4. To test or not to test, Is that a question?
5. How to scale Covid Testing in India
6. Risk and Immunity Report on Covid by Mapmygenome