Runaway Heart: The Long and Short of Long QT Syndrome
Jan 19, 2018
4259 Views
As teenagers, most of us have felt our heart racing or skipped a heartbeat at even the mere thought of our crushes. While most of these “physiological effects” of “being in love” are normal, genetics is a wild card in the general normalcy of life. One such inherited condition associated with irregular heartbeats is Long QT Syndrome.
What is Long QT syndrome?
Long QT Syndrome or LQTS is an inherited genetic condition that causes individuals to have an irregular heart rhythm or arrhythmia. Abnormal heart rhythms can cause episodes of fainting, often during strenuous exercise (e.g., swimming, running), or when experiencing strong emotions (e.g., anger or fear) and, in some cases, can even be life-threatening. It is estimated that about 1 in 2,000 people experience LQTS. However, it is very likely that this estimate may be lower than the actual incidence of LQTS for two reasons:
- Some people with LQTS never experience any symptoms and may remain undiagnosed
- Some people experience sudden deaths— often in their sleep — related to the heart without ever receiving a diagnosis of LQTS (that could have otherwise been life-saving)
Before we get into the details of LQTS, let’s first understand how our heart functions. The chambers of our heart contract and relax to pump blood at each beat. This contraction and relaxation is responsible for efficient blood circulation, and is controlled by electrical signals.
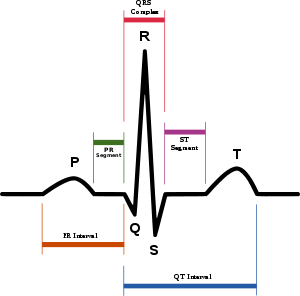
After each heartbeat, our heart recharges itself to prepare for the next beat. These electrical signals travel to our skin and can be measured by electrocardiogram or ECG. ECG is measured as five distinct waves labeled as P, Q, R, S and T. In LQTS, a specific part of this pattern known as the QT interval is abnormally long, which happens when our heart takes more time to recharge between rhythmic heartbeats.
What are the symptoms of LQTS and when do they occur?
The most common symptom of LQTS is fainting spells that can happen without warning. During a normal fainting spell, you may experience initial signs such as lightheadedness, heart palpitations or blurred vision. However, in LQTS when fainting is triggered due to irregular heart rhythms it can be without any warning. Some people may also experience abnormal fast heartbeats or tachycardia. In some cases, when the heart is unable to return to its normal rhythm or an external defibrillator is not used to bring it back to its normal rhythm, a cardiac arrest could lead to sudden death. While most symptoms may be triggered by exercise, emotional stress or auditory stimuli such as sudden loud noises; some people may experience these symptoms in their sleep.
Seek out medical/genetic expertise if you have:
- Sudden blackouts or unexplained fainting episodes
- Rapid heart beats (tachycardia)
- A family member who has experienced sudden blackouts or tachycardia
- Family history of sudden deaths in apparently healthy individuals
People with LQTS can experience symptoms through infancy to middle age but most commonly people experience symptoms like fainting and irregular fast heartbeats in their pre-teen years or in their 20s. Cardiac events are less likely after age 40 years and if present, may be triggered due to use of certain medications or hypokalemia (low potassium in the body).
Some individuals in addition to cardiac concerns may have other features like muscle weakness, unique facial features and physical abnormalities (Andersen-Tawil syndrome); hand/foot and other neurodevelopmental features (Timothy syndrome); or profound hearing loss (Jervell and Lange-Nielson syndrome).
What causes Long QT syndrome?
Inherited LQTS
Inherited LQTS can be caused due to disease-causing changes (mutations) in any of the 15 genes known to be associated with LQTS. About 75% of LQTS are due to known genetic causes. The three most commonly associated genes with LQTS are KCNQ1, KCNH2, and SCN5A. Other genes known to be associated with LQTS are ANK2 (LQT4), KCNE1 (LQT5), KCNE2 (LQT6), KCNJ2 (LQT7), CACNA1C (LQT8), CAV3 (LQT9), SCN4B(LQT10), AKAP9 (LQT11), SNTA1 (LQT12), KCNJ5 (LQT13), CALM1 (LQT14), and CALM2(LQT15).
Acquired LQTS
Certain medications, medical conditions such as low potassium in the body or use of illicit drugs can alter the length of the QT interval causing acquired LQTS. Acquired LQTS may not be caused due to inherited genetic changes.
Does Long QT Syndrome run in families?
Yes, LQTS can be hereditary, meaning it can run in families. LQTS is typically caused due to a mutation in a single gene that may be inherited from either parent.
A specific disease subtype, Jervell and Lange-Nielsen syndrome, which is associated with profound hearing loss in addition to LQTS, is inherited in an autosomal recessive pattern. In such cases, individuals will inherit two mutations; one from each parent.
When LQTS is caused due to a genetic change in one of the genes, it can be passed on to the next generation. It is essential to pass on this information to at-risk family members (siblings, children, parents). Couples who are planning a family will benefit from speaking with a genetic counselor about their reproductive options.
How can genetic testing help with the diagnosis of Long QT syndrome?
Often times, LQTS may be undiagnosed or wrongly diagnosed; it may be important for you to seek an expert in inherited cardiac disorders. Initially, your physician may recommend ECG to look for abnormalities in heart rhythm. A genetic counseling evaluation can be imperative in identifying your risk for LQTS based on personal and family history information. You may be asked to consider genetic testing.
Genetic testing can play a crucial role in establishing a diagnosis of LQTS by:
- Identifying the disease-causing changes in genes that are associated with LQTS
- Differentiating between the types of LQTS
- Personalizing your risk and guiding therapies based on the mutations identified
- Providing information to other at-risk family members
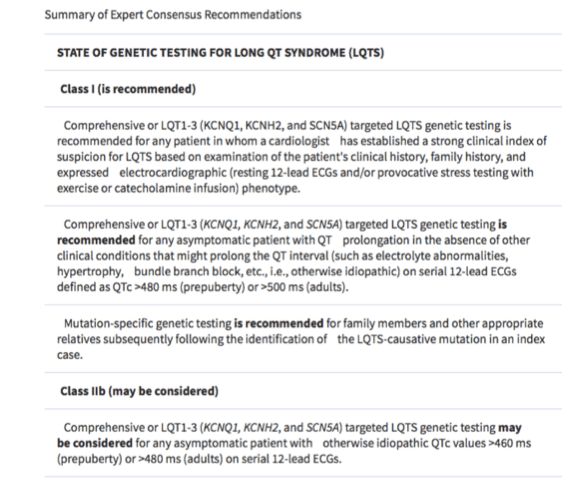 Source: HRS/EHRA Expert Consensus Statement on the State of Genetic Testing for the Channelopathies and Cardiomyopathies: This document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA) (EP Europace, Volume 13, Issue 8, 1 August 2011, Pages 1077 -1109, https://doi.org/10.1093/europace/eur245)
Source: HRS/EHRA Expert Consensus Statement on the State of Genetic Testing for the Channelopathies and Cardiomyopathies: This document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA) (EP Europace, Volume 13, Issue 8, 1 August 2011, Pages 1077 -1109, https://doi.org/10.1093/europace/eur245)
Are treatments available for LQTS?
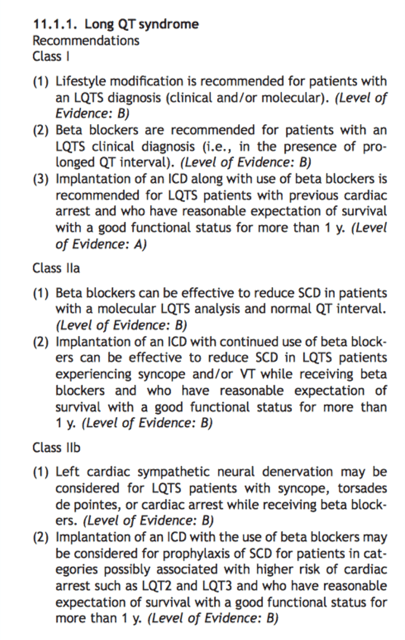
Yes, medications like beta-blockers are available for individuals diagnosed with LQTS. In some cases, a pacemaker or ICD may be recommended to stabilize heart rhythms.
If your LQTS is acquired due to use of medications or other health conditions, your doctor will review your medical history to recommend changes to your medications and lifestyle.
What are some preventative steps I can take if I am diagnosed with LQTS?
If you have been diagnosed with LQTS:
- Speak with your doctor about the medications you plan to take as some medications including common antibiotics, decongestants, anesthetics can cause an increase in QT interval which can result in irregular heart rhythms
- Avoid electrolyte imbalances which can occur due to diarrhea, vomiting or other illnesses
- Lifestyle modifications such as avoiding strenuous exercise, swimming with supervision; reducing exposure to sudden loud noises like alarms or phone ringing can reduce the risk of a cardiac event
 Source: ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) Developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society (EP Europace, Volume 8, Issue 9, 1 September 2006, Pages 746–837, https://doi.org/10.1093/europace/eul108)
Source: ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) Developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society (EP Europace, Volume 8, Issue 9, 1 September 2006, Pages 746–837, https://doi.org/10.1093/europace/eul108)
Who are at risk for LQTS?
- Children, teenagers, or young adults with unexplained sudden fainting spells, unexplained seizures or a history of cardiac arrest
- Family members of children, teenagers or young adults with unexplained sudden fainting spells, unexplained seizures or a history of cardiac arrest
- Family members of people with known LQTS
- People taking medications that alter the QT interval and people with low potassium or other electrolytes
Where can I seek help?
A diagnosis of LQTS can be helpful in guiding therapies and providing essential information for family members. However, receiving a diagnosis can often cause anxiety, fear due to uncertainty or guilt of passing genetic changes to the next generation. Many of these emotions are a normal part of coping with a new diagnosis.
Speaking with a genetic counselor can help you to better understand the diagnosis and discuss emotional and medical implications for yourself and your family members. A genetic counselor is a specialized health care professional who has expertise in medical genetics and psychological counseling. During your genetic counseling session, your risk will be assessed based on your personal and family history and your genetic counselor will recommend appropriate testing. It is essential for you to follow-up with your cardiologist to receive appropriate management guidelines.
If you or your physician are concerned about the possibility of Long QT syndrome, or you or a family member have been recently diagnosed with Long QT syndrome, speak to a genetic counselor today! CALL US on 1800 102 4595 (toll-free) or 040-66986700 or WRITE TO US at info@mapmygenome.in to set up a genetic counseling appointment.