Colorectal Cancer Awareness
Mar 26, 2018
5540 Views
When was the last time you paid attention to your bowel movements? We tend to not pay attention to such activities until there seems to be a problem with it, but our gastrointestinal health influences our overall health as well as our risk of developing various diseases including colorectal cancer.
What is colorectal cancer?
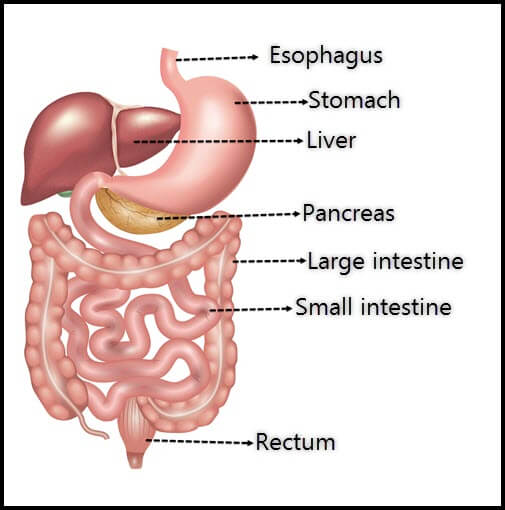
Let’s begin answering that question with understanding what the colon is. The colon is the largest part of the large intestine that ends as the rectum and anus.
Colorectal cancer is cancer of the colon and rectum, is one of the most common cancers worldwide, and affects both men and women. The lifetime risk (risk of developing cancer through age 80 years) of developing colon cancer is about 1 in 22 (4.5%) for men and 1 in 24 (4.15%) for women.
Why should we pay attention to colon health?
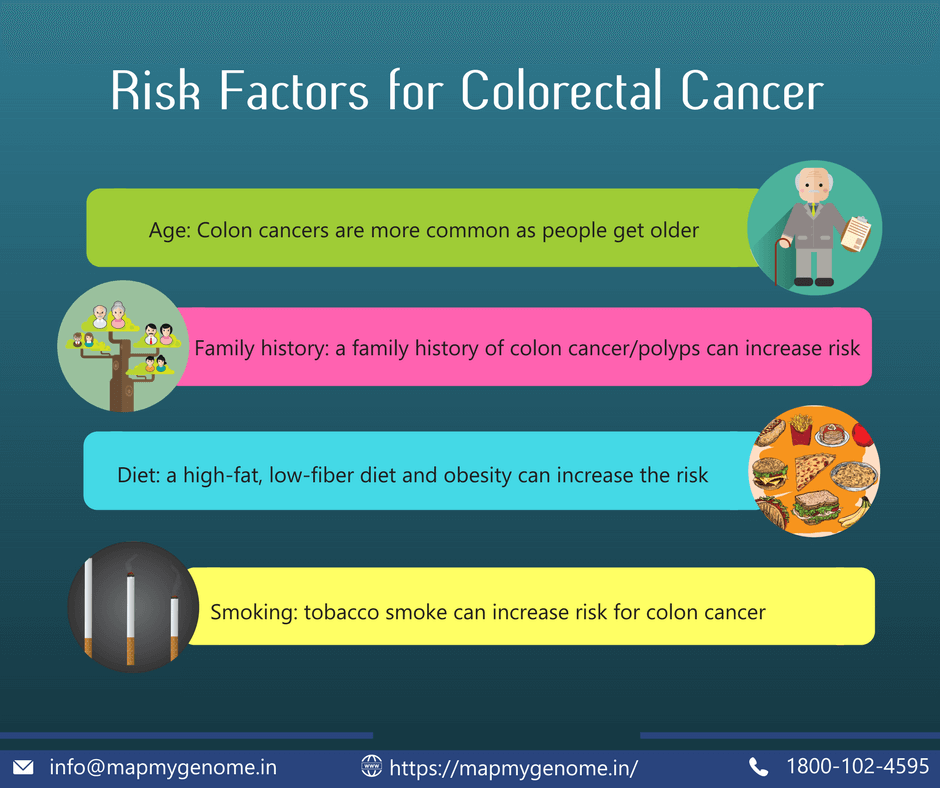
Modifiable risk factors for colon cancer include our diet and lifestyle. It is estimated that about 50–75% of colorectal cancers can be prevented through lifestyle changes such as healthy eating, healthy weight, and exercise. In fact, studies have identified a strong association between weight, exercise, diet, and the risk for colon cancer.
What can you do to improve your colon health?
- Reduce consumption of red meats and processed meats. Increased consumption of red meat is associated with increased risk for colon cancer. In addition, preservatives in processed meat and food can increase risk for cancers.
- Avoid excessive sugar. High sugar consumption can cause weight gain and obesity which is a risk factor for colon cancer. High-sugar and low-fiber diet can lead to ulcerative colitis and Crohn’s disease. Such chronic conditions can, in turn, increase the risk for colon cancer in the future.
- Eat more fiber. Increasing fiber intake can improve overall intestinal and colon health. Adding fiber through fruits, vegetables, whole grains, and legumes can help.
Colonoscopy: Screening can be lifesaving!
A powerful way to prevent colon cancer is through screening. While we all have a risk of developing polyps (abnormal growth in the lining of the colon), sometimes, these polyps may turn cancerous. Colonoscopy is the examination of the colon in order to screen for precancerous growth and remove them during the procedure. A colonoscopy may also detect colorectal cancer early which can help in faster and efficient treatments. The 5-year survival for individuals who have localized cancer (meaning cancer is found where it primarily started or also known as Stage1) is 90%!
For the general population, it is recommended to start colonoscopy at the age of 50 years and repeat it at least every 10 years; earlier, if required, due to clinical or family history reasons. Age of first colonoscopy and frequency of colonoscopy can vary for individuals with a prior personal or family history of colon cancers.
Keeping an eye out
If we can catch the symptoms early, we can successfully treat or prevent cancer. Watch out for the following symptoms:
- Change in bowel habits, e.g. diarrhea, constipation or change in stool consistency for over four weeks
- Rectal bleeding or blood in your stool
- Persistent abdominal discomfort such as cramps, gas, or pain
- A feeling that your bowel doesn’t empty completely
- Weakness or fatigue
- Unexplained weight loss
Hereditary colon cancers syndromes
Most cancers up to 80% are sporadic, which means they occur in older ages (>60 years) and are mostly caused due to combinations of many risk factors such as age, diet, and lifestyle. About 15-20% of cancer are familial, which is why we may see clusters of cancer in the family but may not be able to identify a significant pattern of history or underlying genetic factors. Only about 5-10% of colon cancers are caused due to underlying genetic changes that increase the risk of developing cancer. Disease-causing changes in certain genes can cause susceptibility to colon cancer. Individuals with hereditary colon cancers may present with multiple polyps, may have few polyps or have no polyps.
Lynch Syndrome
One such common hereditary colon cancer syndrome is Lynch Syndrome a.k.a. Hereditary Non-Polyposis Colon Cancer. Typically, individuals with Lynch syndrome present with less than 10 pre-cancerous polyps in their colon. Families with Lynch syndrome have early onset colon cancer (usually under the age of 50 years); women in such families may also have uterine or ovarian cancer. We also see a higher rate of incidence of prostate cancer in men from families with Lynch syndrome. Lynch syndrome is caused due to disease-causing changes (mutations) in any one of five genes (MLH1, MSH2, MSH6, PMS2, and EPCAM).
Polyposis Syndromes
Individuals with hereditary colon cancer syndromes caused due to mutations in genes such as APC or MUT-YH present with multiple polyps. In some of these cases, the colon may be carpeted with over 100 polyps! In Familial Adenomatous Polyposis (FAP), which is caused due to mutations in the APC gene, individuals present with early onset colon cancer, typically in their 40s. In addition, we may note other rare cancers such as jaw-bone cancers.
In contrast, there is a lot of variability in families with mutations in MUT-YH gene. While some may not have a strong presentation of cancer or may typically present with cancers in their 60s or 70s; others may present with cancer in their 40s or with multiple polyps.
Colon cancer is a largely treatable condition in about 95% of cases. Families and individuals with hereditary colon cancer syndromes can reduce the risk of developing cancer or even prevent cancer via regular screening and risk-reducing strategies involving dietary and lifestyle modification. For some families, preventative surgery may also be an option.
The cancer was ‘down there’
It is not uncommon in families to be not aware of the origin of cancer diagnosis. This may be due to the late diagnosis of cancer when the disease is in advanced stages. Often, diagnosis of reproductive tract cancers, such as ovarian or uterine cancer is misinformed as ‘stomach’ cancers. This can create many challenges, including the inability to provide accurate screening recommendations for other family members. Lack of accurate information for family members may also lead to misdiagnosis or undiagnosed genetic causes of cancers.
Red flags for genetics include:
- Colon cancer under the age of 50 years
- Personal history of polyps (greater than 10)
- Multiple cancer diagnoses in the family; for example, colon, uterine, prostate and brain cancer
- Three or more generations with cancer history
- Two people in the same generation with colon or uterine cancer
Genetic testing and counseling can help prevent cancers!
If you (or someone in your family) observe any of the above red flags, you will benefit from speaking with a genetic counselor who will assess your medical and family history, and help you understand any possible underlying genetic causes of cancer, if present. Genetic testing can identify specific genetic causes for cancer that can help families personalize screening and treatment recommendations.
Speaking with a genetic counselor can help you to better understand your risk as well as help discuss and address emotional and medical implications for yourself and your family members. A genetic counselor is a specialized health care professional who has expertise in medical genetics and psychological counseling.
If you are concerned about your medical center history or family history, and would to set up a genetic counseling appointment, CALL US on 1800 102 4595 (toll-free) or 040-66986700 or WRITE TO US at info@mapmygenome.in OR book an appointment online with one of our awesome genetic counselors.
References
https://seer.cancer.gov/statfacts/html/colorect.html
https://www.cancer.net/cancer-types/colorectal-cancer/introduction

