What We Learned from Irrfan Khan
Apr 04, 2018
5325 Views
Most of us have read these words from Irrfan Khan:
“The last fifteen days, my life has been a suspense story. Little had I known that my search for rare stories would make me find a rare disease. I have never given up and have always fought for my choices and always will.”
As a genetic counselor, I feel strongly about destigmatizing health issues, and Irrfan Khan has shown us all that health and illness can both be talked about with honesty and respect. Bollywood is a great influencer – in ways good, bad and ugly – and our leading actors like Deepika Padukone, Amitabh Bachchan, and Irrfan Khan have led by example in normalizing conversations about illnesses such as anxiety and depression, tuberculosis, and cancer. Irrfan promised he would post an update about his diagnosis, and he did. With grace and dignity. This was, for many people (including Irrfan), the first time hearing/reading the term neuroendocrine tumor (NET). Irrfan’s inherent spirit and wit are clearly unfazed by his diagnosis as he took a light stab at rumors about a brain condition thanks to the term ‘neuro’, and half-jokingly introduced rumor mills to the cutting-edge concept of fact-checking. So let’s get some facts straight.
What is a neuroendocrine tumor?
If you’ve heeded Irrfan’s advice and done a quick search on Google, you already know that neuroendocrine tumors (NETs) are abnormal growths that originate from the cells of the endocrine (hormonal) and nervous systems. While many NETs are benign (non-cancerous), some are malignant (cancerous). NETs typically occur in the intestine, where they are called carcinoid tumors; however, they are also found in the pancreas, lung and the rest of the body.
What are the symptoms of NET?
Given that there are several different types of NETs, they may cause different symptoms. This depends on the tumor location, and whether the NET is functional or nonfunctional. Functional NETs may lead to clinical symptoms, because the tumor causes excessive hormone secretion. Nonfunctional NETs do not secrete hormones but may produce symptoms because of growth of the tumor itself.
Some common symptoms of NETs include1:
- Flushing (redness, warmth) on the face or neck without sweating
- Diarrhea, including at nighttime
- Shortness of breath, rapid heartbeat/palpitations
- High blood pressure
- Fatigue, weakness
- Abdominal pain, cramping, feeling of fullness
- Unexplained weight gain or loss
- Wheezing, coughing
- Swelling in the feet and ankles
- Skin lesions, discolored patches of skin, thin skin
- High blood glucose levels (frequent urination, increased thirst, increased hunger)
- Low blood glucose levels (shakiness, dizziness, sweating, fainting)
Oftentimes, NETs do not cause symptoms at the early stages. Further, as you may have noticed from the list above, when symptoms do present, they may be similar to those caused by more common conditions. Consequently, NETs can be misdiagnosed as Irritable Bowel Syndrome (IBS). An important distinction that the abdominal discomfort of IBS is usually relieved by a bowel movement. If you notice new or persisting symptoms or changes in your body, let your doctor know.
Why am I reading about NETs on a genetics-related website?
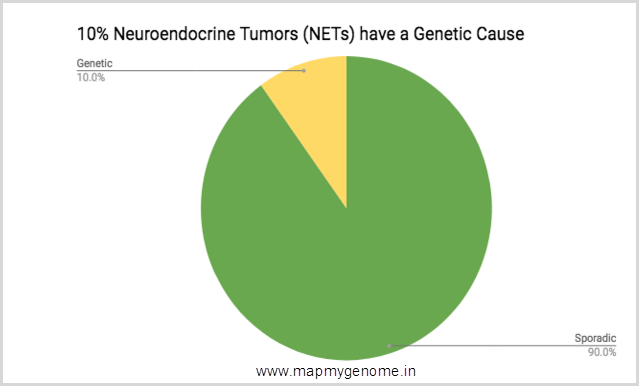
Good question. While the majority of NETs are sporadic, certain inherited genetic disorders and chromosomal abnormalities are known to be associated with a predisposition (or susceptibility) for developing NETs and other tumors. Individuals with a genetic predisposition can benefit from genetic testing that can help identify their risk for tumors that can be screened. Screening leads to early detection and better survival rates. While most individuals diagnosed with cancer receive appropriate treatment for cancer they have been diagnosed with, the lack of awareness of and/or access to genetic testing keeps them from receiving an important plan for risk-reduction and screening for the other tumors they may be at increased risk for. This is, sadly, a big loss in the window of opportunity for screening, early detection and/or prevention. In fact, about 10% NETs are associated with an inherited condition. That’s 1 in every 10 individuals diagnosed with a NET!
Here are the two important inherited conditions known to be associated with NETs:
I. MULTIPLE ENDOCRINE NEOPLASIA
The most common inherited genetic condition associated with NETs is Multiple Endocrine Neoplasia – Type 1 (MEN 1). MEN 1 is a syndrome characterized by pancreatic, parathyroid, and pituitary endocrine tumor. Sometimes, patients with the MEN 1 syndrome may develop NETs or a carcinoid tumor, adrenal tumors, and tumors of the ovaries and thyroid. About 30-60% of patients with MEN1 will develop a neuroendocrine tumor (NET). MEN 1 syndrome is known to be caused by changes in the MEN1 gene on chromosome 11. MEN1 gene changes can be seen in males and females, and an individual who carries a gene change in the MEN1 gene is said to have a genetic predisposition for developing a MEN1-related neoplasm. This pattern of inheritance is consistent with an autosomal dominant trait. This means that an affected individual has a 50% chance of passing it on to each of his/her children (son or daughter).
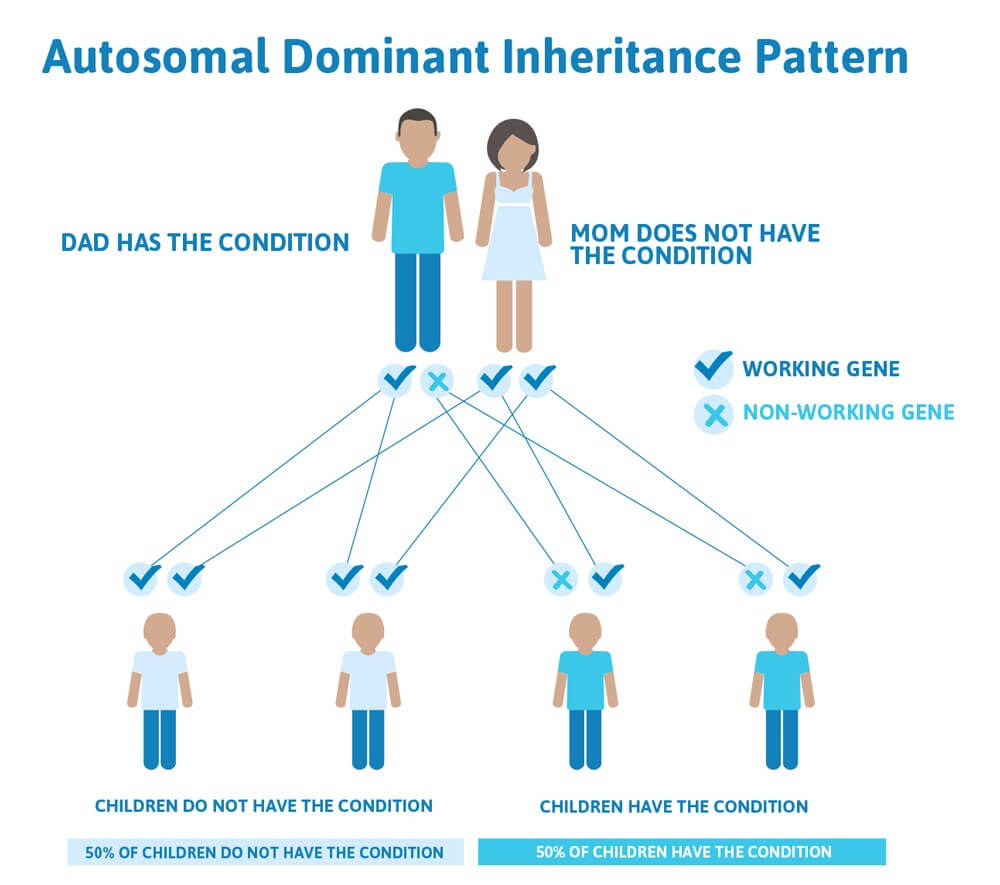
Image source: https://geneticsupportfoundation.org/archive/genetics-and-you/autosomal-dominant-inheritance
II. VON HIPPEL-LINDAU DISEASE
Less common than the MEN 1 syndrome is von Hippel-Lindau disease (VHL), a syndrome characterized by visceral cysts (cysts in internal organs) and benign (non-cancerous) tumors with the potential for turning malignant (cancerous). Tumors of the pancreas/kidney and cysts of the kidneys or liver are also associated with VHL. Loss of vision is a very common manifestation of VHL, and other organs can be affected as well — strokes, heart attacks, and cardiovascular disease are common additional symptoms. VHL is caused by changes in the VHL gene on chromosome 3; the inheritance for VHL is also considered to be autosomal dominant. About 11-17% of patients with VHL will develop a NET.
| GENETICS and NETs |
|
|
|
I am now concerned about my risk. What should I do?
It is normal (and appropriate) to be concerned if you or a family member has been diagnosed with a NET. In the information age, ignorance is NOT bliss. In fact, knowledge is power. Learning about your risk can seem scary at first, but putting together a proactive plan focused on prevention, risk-reduction, and screening is powerful. Here’s what you can do:
- Gather as much information about your medical history and/or family history as possible (ages of onset, type of tumor, etc.)
- Get this information for BOTH sides of your family — you get half your genes from your Mom’s side and the other half from your Dad’s side
- Make a list of questions and concerns you have
- Set up an appointment to speak with a Genetic Counselor who will address your concerns, make an accurate risk-assessment, discuss testing options, help you strategize a plan for testing/screening, and help you cope with the medical and emotional implications of any new and unexpected information.
Genetic Counselors are experts with specialty training in medical genetics and psychological counseling.
The unexpected makes us grow
Thank you for sharing what I can only imagine must have been a difficult time in your life, Irrfan. You’re right — The unexpected can certainly make us grow, no matter how scary it might seem at first. Don’t ever give up; continue to be the warrior that you are, and we hope to talk to you about your journey in health and resilience. I hope your honesty and authenticity spark a meaningful discussion about how we speak about health, illness, and recovery. We wish you a speedy and complete recovery. Here’s a nerdy riddle for you:
Q: What’s a neuroendocrine tumor?
A: That’s a no-brainer!
How can I schedule an appointment with a Genetic Counselor?
If you would like to set up a genetic counseling appointment to discuss your medical history and/or family history, CALL US on 1800 102 4595 (toll-free) or 040-66986700 or WRITE TO US at info@mapmygenome.in. You may also book an appointment online with one of our awesome genetic counselors.
References
- https://www.cancercenter.com/neuroendocrine-tumors/

