Simplifying Blood Tests for Covid
May 10, 2021
48244 Views
Almost all of us have done a blood test at some point in our life. Whether it is for a general checkup or a specific problem, it is critical to understand the purpose and limitations of the tests we do. This series will simplify those for you. In this blog, I am writing about COVID-19 specific blood tests.
Given that getting an RT-PCR may be difficult or getting reports are taking time, there are some blood tests that can help your doctor determine if you have been exposed to the SARS-Cov2 virus or how severe it is. Antibody tests (IgG, IgM and Neutralizing Antibodies) that we have discussed previously are helpful to understand if you developed antibodies to the infection. Of course, currently, some of these blood markers are also hard to find given the surge in cases in India.
The most commonly prescribed blood tests when a doctor suspects COVID or you are COVID positive are the following. An HRCT scan is also usually recommended.
- CRP C reactive protein
- CBC Complete Blood Picture
- Lactate Dehydrogenase (LDH) Test
- D Dimer
- Interleukin 6
- LFT: Liver Function test
- Ferritin
- Serum Creatinine
Some of these tests are the ones you may have done when you got a health checkup. Some specific ones look at inflammation like CRP and IL-6. D-Dimer looks at blood clots. So what is the significance of each of these tests?
CRP: C- Reactive Protein
This is a blood test to help detect the presence of inflammation or an infection. For COVID, this is a commonly used blood marker as increased levels may reflect infection spreading in the body. The C-reactive protein is made by the liver in response to inflammation, but elevated levels do not specify where the inflammation has occurred. If you don’t have a chronic illness, this may be a good indicator of a recent infection such as COVID. This happens quickly (within hours) and can increase a thousand fold also. This may be prior to other symptoms someone may see, as inflammation is our body’s first response to infection.
We may all now be familiar with CRP thanks to its use as a screening test for COVID, this test is often prescribed to monitor patients after surgery, transplant, or to detect sepsis (an infection in the blood), heart attack, etc. Your doctor may order this test if you have tested positive (RT PCR) for COVID. Alternatively, you can get this done if you have symptoms like fever, chills, rapid heart rate, or fast breathing.
For those with autoimmune diseases like Rheumatoid arthritis or Lupus, this is used to assess the effectiveness of the treatment.
Normal Range:
Up to 6 mg/L
When you should be worried? Levels above 10
When to test for CRP?: Other than those hospitalized, it is also recommended by doctors for those isolated at home and symptoms don’t improve within 4-5 days. Normally done twice with a gap of 4-5 days to understand inflammation in the body.
CBC – Complete Blood Picture
Complete Blood Count or CBC is an analysis of the size, number, and maturity of different blood cells in a specific volume of blood. If you remember your high school biology you will remember that our blood has several types of cells like WBC (white blood cells), RBC ( red blood cells) and platelets. When you see an increased number of WBC, it means that the body is fighting an infection. You have also probably heard of platelet count for dengue patients. When platelets reduce, you know it is not a good sign.
- Red blood cells transport oxygen. They fight anaemia and fatigue.
- White blood cells fight infection. Increased WBC count may indicate the presence of an infection. Decreased levels may indicate certain rheumatic diseases or reaction to the medication.
- Platelets prevent bleeding and bruising. Their count is measured to check for a blood infection.
A complete blood picture is the most commonly ordered test as it can give you information on general health and possible infections as well. For COVID, the important parameters to look at would be the eosinophils and lymphocytes.
Eosinophils are one kind of white blood cell that helps fight disease and typically make up to 6% of the blood.
Based on evidence from several articles, it appears that if a COVID positive patient has lower eosinophils and lymphocytes, they are likely to have a longer hospital stay.
Lactate Dehydrogenase (LDH) Test
Lactate dehydrogenase (LDH), also known as lactic acid dehydrogenase, is found in blood or other body fluids. As I had mentioned earlier, since it ends in “ase”, it is an enzyme. LDH is an enzyme that plays an important role in the production of energy for the body. When you have high levels, it means that some infection or disease has attacked your body. It basically means you have tissue damage because of disease or infection. So for COVID, elevated levels can show an active infection. This test is non specific though. There is a different test called LDH isoenzyme test that can help with severity and location and type of tissue damage.
Normal Range:
- Newborns: 160-450 U/L
- Infants: 100-250 U/L
- Children: 60-170 U/L
- Adults: 100-190 U/L
- Non specific: 105-333 IU/L

D Dimer
D-dimer is a fibrin degradation product that is often used to measure and assess clot formation. In COVID-19 patients, elevated D-dimer levels have been associated with disease severity and mortality trends.
Typically these tests are done if you have symptoms of a bleeding/clotting disorder such as deep vein thrombosis, pulmonary embolism, etc., as D-dimer is produced when a blood clot is dissolved. Normally the levels are very low unless there is an injury or infection. These levels may rise sharply in the case of COVID.
You must have heard the term hemorrhage connected with brain hemorrhage, etc. That occurs when blood is lost to bleeding. The opposite of that is hemostasis, that is the body’s mechanism to create a clot to prevent bleeding and maintain stability. So when a blood vessel or tissue is injured, blood-based hemostasis is initiated with the production of a protein called fibrin. Fibrin, being a fibrous protein, forms crosslinks to form a fibrin net much like Spiderman spinning a web with platelets to hold the forming blood clot in place near the injury site till it can heal.
Once it starts to heal, then the body uses an enzyme called plasmin to break the clot so it goes away. What remains of the fibrin now are fibrin degradation products (FDP) which have many sizes of the cross-linked fibrin. One of the by-products of the breakdown of fibrin is D-dimer, which we can measure in your blood sample. This level can be very high when many clots are formed and broken. I imagine many of us have heard of ‘blood clots’ and ‘COVID’ said in the same sentence many times this year. Understandably, this is therefore an important parameter to look at. There can be many more reasons to have increased levels of D-dimer as mentioned above.
Normal Range:
<500 ng/mL
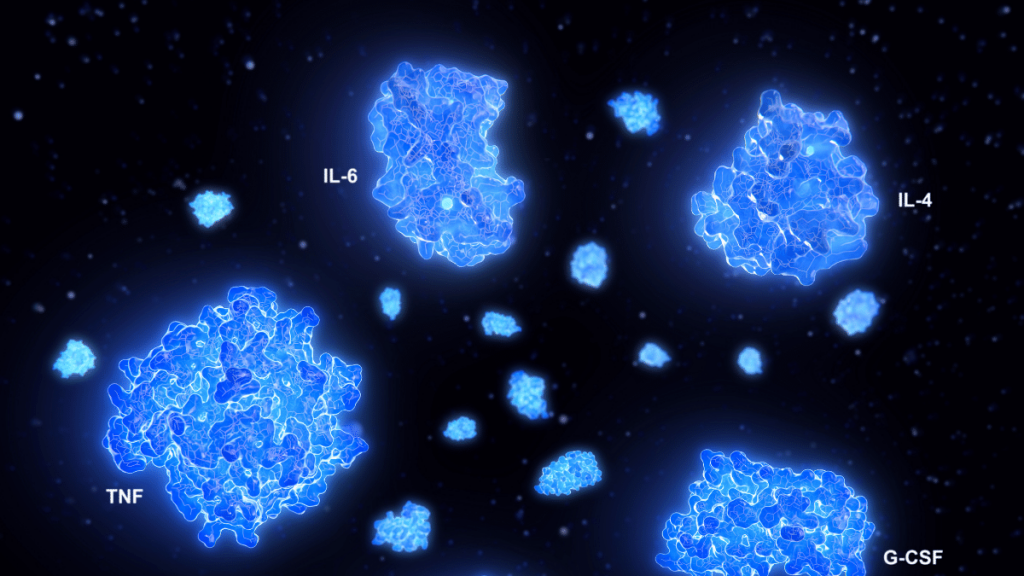
Interleukin 6
I first heard of IL 6 many years ago when we were working with a group working on ALS. This is a fascinating cytokine- a protein produced by certain immune cells during inflammation or tissue injury. This is a reaction by both our innate and adaptive immunity (if you remember those from previous blogs). From our innate immunity perspective, IL6 is a very potent pro-inflammatory cytokine It first goes to the liver and attacks the hepatocytes (hepato means liver) which in turn shows an increase in several markers like CRP (discussed above), fibrinogen (cardiac disease), hipcidin (anemia of chronic disease), increased platelet count and more. You get the picture.
IL6 in the adaptive immunity allows antibody-producing B cells to proliferate, leading to an enhanced antibody response. IL6 can be found in patients who have localised infections, chronic inflammatory diseases like rheumatoid arthritis or infections like Covid 19.
An interesting thing to note is that Tocilizumab, an antibody that blocks IL-6 function by binding to the IL-6 receptor, that has been used for inflammatory diseases like RA has been useful for Covid patients as well.
IL6 is not very stable if the sample is not properly stored or used after 24 hours.
Normal Range:
0-16.4 pg/mL
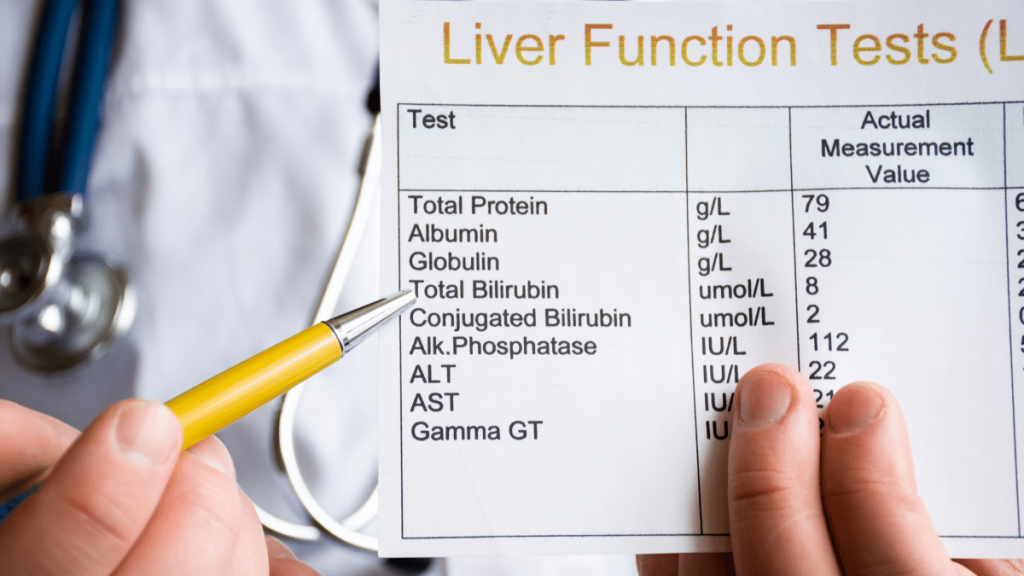
LFT – Liver Function test
The liver filters and processes the blood circulating throughout the body. The liver performs several vital functions including metabolizing nutrients, detoxification of harmful substances, and production of blood clotting proteins. The liver achieves this due to proteins it contains called enzymes that drive these chemical reactions. In the case of liver injury, the cells get damaged or destroyed, leaking these enzymes into the bloodstream, which are measured through such tests indicating possible liver injury. The two main enzymes tested are SGOT and SGPT.
Aspartate aminotransferase (AST), SGOT: This enzyme is also found in muscles and several other tissues other than the liver.
Alanine aminotransferase (ALT), SGPT: ALT is found almost exclusively in liver cells only. Elevated levels of both ALT and AST together in the bloodstream indicate liver damage.
Alkaline phosphatase (ALP) and GGT: Another key function of the liver is the production of bile, which is necessary for fat digestion. Bile flows through the liver through small tubes (ducts) and eventually gets stored in the gallbladder under the liver. If bile flow is slow or restricted, the blood levels of certain liver enzymes increase, prime amongst which is ALP followed closely by GGT. Elevated ALP levels indicate a problem with the bile flow, which may be caused by a problem in the liver, the gallbladder, or the ducts. Gamma Glutamyl Transferase (GGT) is an enzyme found in several organs, but has the highest concentration in the liver. Increased levels of GGT in the blood also indicate liver injury, and in combination with increased ALP levels allow a diagnosis of the same.
Bilirubin: Bilirubin is a yellowish pigment found in bile and is a metabolic byproduct of heme catabolism. Bilirubin is excreted in bile and urine, and elevated levels give a distinct yellow colouration associated with jaundice. Elevated levels can be due to increased bilirubin production (indicating hemolysis and ineffective erythropoiesis), decreased bilirubin excretion (indicating obstruction and hepatitis), abnormal bilirubin metabolism (indicating neonatal or hereditary jaundice). Direct (conjugated) bilirubin is elevated more than indirect (unconjugated) bilirubin in viral hepatitis, drug reactions, alcoholic liver disease, bile duct blockage (indicating possible gallstones), tumors and scarring of bile ducts. Indirect bilirubin is more elevated than direct bilirubin in cases of pernicious anemia, transfusion reaction and metabolic conditions such as Gilbert syndrome.
Normal Range:
ALT: 7-56 units/L
AST 10-40 units /L
Ferritin
Ferritin is a blood protein that contains iron. A ferritin test helps your doctor understand how much iron your body stores. As Dr Krishnam Raju, a well-regarded cardiologist and researcher explained to me, low Ferritin means that your bank balance of iron is low in the body. Now, why is that important? When there is a cytokine storm in your body, these levels will be unusually high. Your doctor can help understand if your body has been attacked by a cytokine storm and suggest next steps.
Normal Range:
23.9-336.2 ng/mg

Serum Creatinine
Serum Creatinine test measures the creatinine levels in the blood. Creatinine is a byproduct of energy production in the muscles. Creatinine enters and exits the bloodstream at a constant rate. The kidneys filter and help in elimination of creatinine. Higher levels of serum creatinine may indicate poor kidney function or kidney damage.
Impaired kidney function is often associated with COVID. Some studies suggest that COVID patients are at a higher risk for acute kidney injury. Your doctor may recommend a serum creatinine test to assess kidney health.
Normal Range:
♂ 0.74 to 1.35 mg/dL
♀ 0.59 to 1.04 mg/dL
We hope you found this article useful. In COVID times, stay healthy, stay safe, and stay informed!

