Chadwick Boseman, Colorectal Cancer, and Awareness
Sep 08, 2020
5976 Views
Chadwick Boseman, the star of the 2018 Marvel Studios mega-hit Black Panther, died of colon cancer last Friday. He was 43 years, diagnosed 4 years ago, and had kept his condition a secret. His death came as a shock to the world, but has put the spotlight on colon cancer, understanding one’s risks, education about early symptoms, and the importance of screening. While most of us are familiar with what cancer is — the uncontrolled growth of abnormal cells anywhere in a body — colon cancer may be slightly unfamiliar to most. So what is colon cancer?
Colon cancer, as the name suggests, is the growth of cancer cells (or malignant cells aka tumor cells) in the colon. Colon cancer and rectal cancer are often grouped together because they have many features in common, and are commonly referred to as colorectal cancer. They are distinguished from each other as either colon cancer or rectal cancer, depending on where the cancer originated — the colon or the rectum. If you don’t know what the colon or the rectum is, don’t worry. To understand colorectal cancer, it is important to understand what the colon and the rectum are, what they do. We’ll get to the bottom (pun unintended) of this right away.
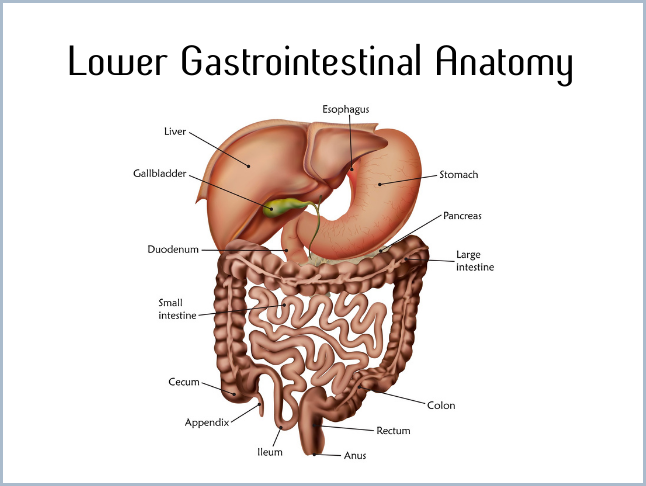
The colon and the rectum are part of your large intestine which, in turn, is part of your digestive system. The digestive system is often referred to as the gastrointestinal (GI) tract, and colorectal cancer (CRC) is a common GI tract cancer. The large intestine is a muscular tube, about 5 feet long and mostly made up of the colon, whose job is to absorb water and salts from the food and water that pass through our digestive system. The nutrients from the food we eat are absorbed by the small intestine before it gets pushed along into the large intestine where the colon does the important job of final absorption before passing on the waste matter into the rectum. The rectum is different from the anus. The rectum is the final 6 inches of the digestive tract where waste matter is stored before it can get passed out of your body through the anus. Luckily, we have a ring of muscles — called a ‘sphincter’ — around the anus, which keeps the stool from coming out until they relax during a bowel movement. If reading about the anus is embarrassing to you, please know that it’s far more embarrassing to be pooping your pants. Or skirt, or salwar, or saree. The digestive system has no gender. Also, sadly, this kind of “embarrassment”, is a major reason why most people shy away from having conversation and seeking information about colorectal cancer. There is no shame in taking care of your health! Your colon and rectum play an important role in maintaining digestive health, and colorectal cancer is one of the easier-to-detect-and-treat cancers because, in most cases, colon and rectal cancers grow slowly over many years. Conversations, education, and destigmatization are important. Let’s continue.
One of the most important things to remember about colorectal cancer — or any cancer, for that matter — is that it typically starts with the overgrowth of cells. A ‘polyp’ is the term used for the overgrowth of cells that line the colon. While the vast majority of colon polyps do not result in cancer, nearly all colon cancers start in a polyp. Go back; read that sentence again. The most common type of polyp is called an ‘adenoma’— the medical word for a “pre-cancer” kind of overgrowth that can, eventually, grow into a cancer. Luckily, for those of you who understand the life-saving benefits of screening and early detection, an adenoma typically takes years before it can become cancer. So it makes sense that we should look for these polyps/adenomas, right? Right! It’s what we call ‘screening’.
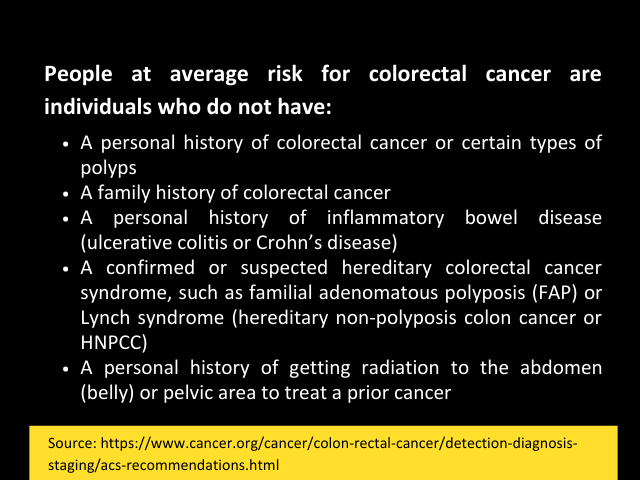
The American Cancer Society (ACS) recommends that people at average risk of colorectal cancer start regular screening at age 45. And while no one really wants to think of themselves as “average”, it can be a “good” thing when you’re talking about cancer risks.
Colorectal cancer screening can be done either with a sensitive test that looks for signs of cancer in a person’s stool, or with an imaging-based exam that looks at the colon and rectum.
| STOOL-BASED TESTS | IMAGING-BASED TESTS |
| Fecal immunochemical test (FIT) every year | Colonoscopy every 10 years |
| Guaiac-based fecal occult blood test (gFOBT) every year | CT colonography (virtual colonoscopy) every 5 years |
| Multi-targeted stool DNA test (mt-sDNA) every 3 years | Flexible sigmoidoscopy (FSIG) every 5 years |
There are some differences between these tests but, without going into details of each of these tests, the most important thing is to get screened, regardless of which test you choose. Speak to your health care provider about which tests might be good options for you. If you choose any screening test other than colonoscopy, it is recommended to follow up any abnormal test with a timely colonoscopy. What’s a colonoscopy? Fair question.
A colonoscopy is a screening tool for colon polyps and cancer. Screening may help find diseases at an early stage, when the success rate of effective treatment is the greatest. Screening is especially important if you notice symptoms of colorectal cancer. Some early symptoms include:
- A change in bowel habits, such as diarrhea, constipation, or narrowing of the stool, that lasts for more than a few days
- A feeling that you need to have a bowel movement that is not relieved by doing so
- Rectal bleeding
- Dark stools, or blood in the stool
- Cramping or abdominal (belly) pain
- Weakness and fatigue
- Unintended weight loss
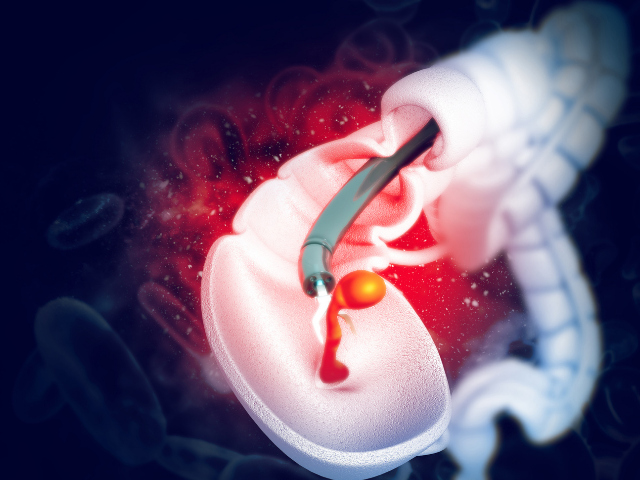
Oftentimes, however, when colorectal cancer does turn out to be the cause, symptoms usually appear after the cancer has spread. It is for this reason that it’s best to test for colorectal cancer even before having any symptoms, through screening. A colonoscopy is the gold standard screening tool for colorectal cancer. During a colonoscopy procedure, a doctor uses a flexible tube with a miniature camera attached to view the inside lining of your rectum and colon. Don’t worry though, most people feel nothing more than slight discomfort during a colonoscopy because mild sedation and pain medication are administered as part of the procedure. It is this procedure that can identify polyps or adenomas (remember those?), which are removed during the colonoscopy itself (you won’t feel this) and sent to a laboratory for analysis to determine whether they are cancerous, pre-cancerous, or non-cancerous (aka benign). If this has been overwhelming, then fear not… this marks the end of the part of this article for those at ‘average’ risk.
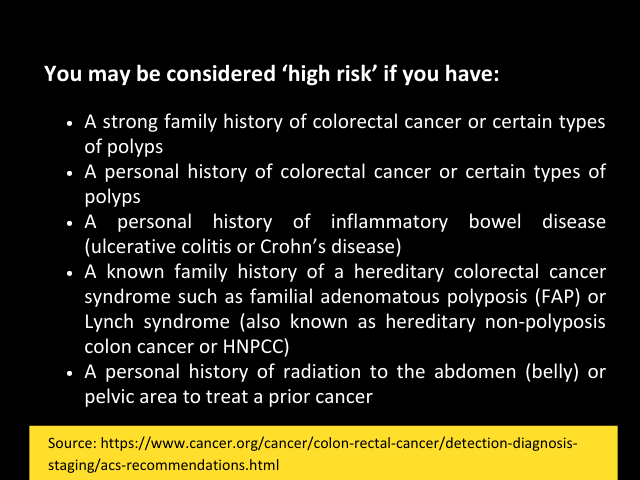
If you’re at increased or ‘high’ risk, the American Cancer Society recommends that you start colorectal cancer screening before age 45 years, be screened more frequently, and/or get specific tests.
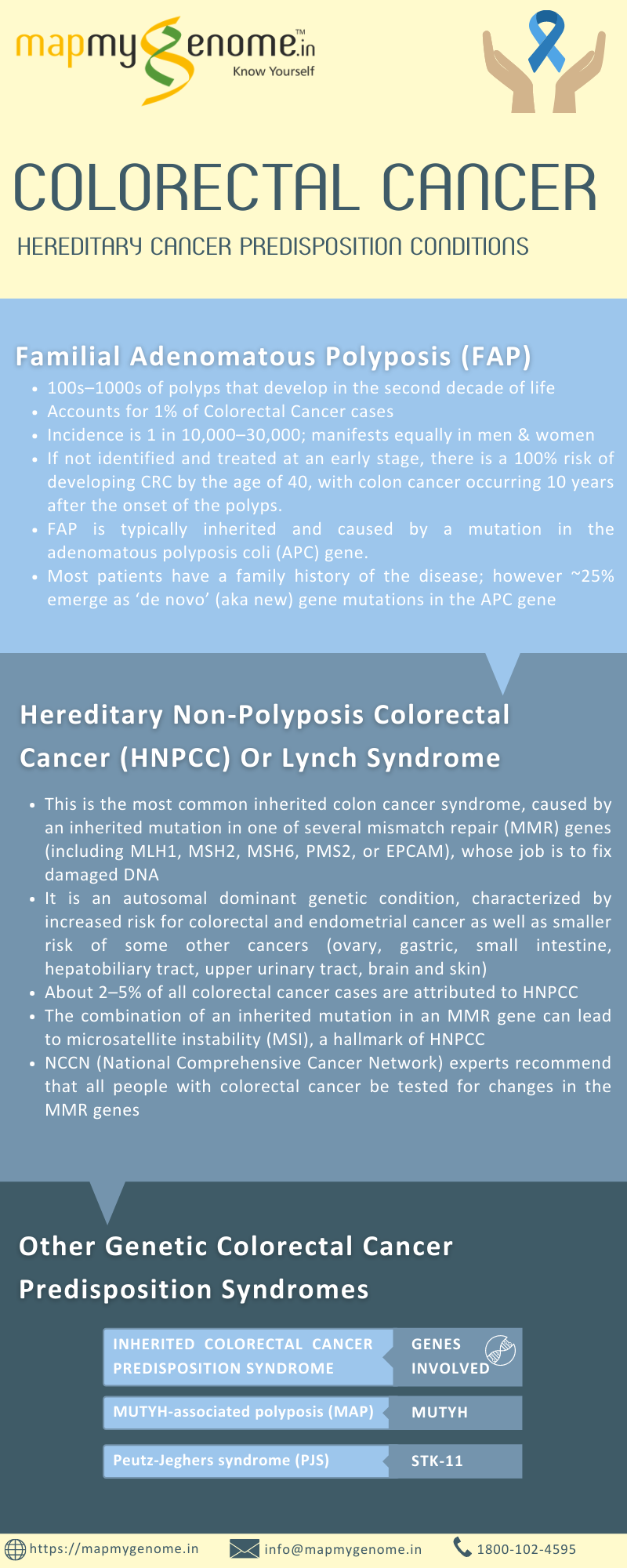
So while most cancers — including colorectal cancer — are sporadic, sometimes, they are caused by inherited changes in genes that can increase cancer susceptibility. For colorectal cancer, two most common hereditary cancer predisposition conditions are FAP (Familial Adenomatous Polyposis) and HNPCC (Hereditary Non-Polyposis Colorectal Cancer).
Family history tends to remain an important aspect of risk assessment for colorectal cancer. A genetic counselor can analyze your family history and medical history in order to help you identify your risk, facilitate genetic testing, and put together an appropriate plan for screening/management, and/or make a referral to a specialist if needed. A genetic counselor can also be a great resource to answer all your questions about cancer, family history, and strategies for risk reduction, as well as to address any fears or concerns you may have about colorectal cancer. The more conversations are had, the more are we able to understand our risks, learn about early symptoms, and put into place a plan for screening that may help early detection and treatment so that we don’t lose more lives like Chadwick Boseman to this screenable, identifiable, and treatable cancer.
You may set up an appointment with a genetic counselor by sending an email to info@mapmygenome.in or calling 1800-102-4595 (toll-free).
About the Author

Pooja Ramchandran is a pioneer in the field of genetic counseling in India and VP Genetic Counseling at Mapmygenome. She has been practicing clinical genetic counseling in India since graduating from Johns Hopkins University in 2008. She is a much sought-after expert in a niche profession and, being the first genetic counselor in the country with a formal degree in genetic counseling, she is committed to establishing the genetic counseling profession in India. When she is not offering her expertise as a genetic counselor, Pooja is a stand-up comedian.