Rebound Hypertension- The Fatal Danger of Abruptly Stopping Beta-Blockers
Feb 13, 2022
17157 Views
It was my second year of medical school. My grandmother had already been diagnosed with hypertension and on medication for decades. My grandmother would ask me to check her medicines and ask me about them, trying to learn more about them. She would always travel places around with her medications. She was experiencing blackouts, nausea, and palpitations which were later diagnosed to be angina. She has been put on beta-blockers (metoprolol) since then to prevent such episodes. She ran out of medication one day and was going to restock it the next day, skipping the medication for that day. Later in the night she developed nausea, dizziness and then was found unconscious. She was taken to the nearby hospital, where we found out her blood pressure shot up and she suffered a stroke, paralyzing her and losing her ability to speak. It was too early for me to understand what went wrong until my professor explained to me the rebound phenomenon. Sadly, her condition deteriorated and she passed away after a few months.
Beta-blockers are the drugs used in the treatment of hypertension, sudden withdrawal of beta-blockers causes rebound hypertension, worsening of angina, and sudden death in some.
WHAT ARE BETA-BLOCKERS
Beta-blockers are beta-adrenergic receptor blockers, which are majorly used to treat cardiovascular diseases and other conditions. They work by blocking beta-adrenergic receptors, which are present in various organ systems.
Beta 1 receptors are usually and largely present in the heart, thereby controlling cardiac activity.
Beta 2 receptors are present in various locations controlling metabolic activities and smooth muscle relaxation.
Beta 3 receptors are present in adipose tissue dealing with fat metabolism.
Beta-blockers act by blocking the adrenergic receptors and are classified into two categories:
- Nonselective beta-blockers -
Ex: Propranolol, Labetalol, Carvedilol, Sotalol, Timolol,Pindolol. - Cardioselective (beta1) -
Ex: Metoprolol, Atenolol, Acebutolol, Bisoprolol, Esmolol, Betaxolol, Celiprolol, Nebivolol.
FDA approved indications for the usage of beta-blockers
- Tachycardia
- Hypertension
- Myocardial infarction
- Congestive heart failure
- Cardiac arrhythmias
- Coronary artery disease
- Hyperthyroidism
- Essential tremor
- Aortic dissection
- Portal hypertension
- Glaucoma
- Migraine prophylaxis
Also used less frequently in
- Long QT syndrome
- Hypertrophic obstructive cardiomyopathy.
- Anxiety
- Reduction in tremors
CARDIOVASCULAR SYSTEM -
The catecholamines, epinephrine, and norepinephrine bind to B1 receptors and increase cardiac automaticity as well as conduction velocity. B1 receptors also induce renin release leading to an increase in blood pressure.
In contrast, binding to B2 receptors causes relaxation of the smooth muscles along with increased metabolic effects such as glycogenolysis.
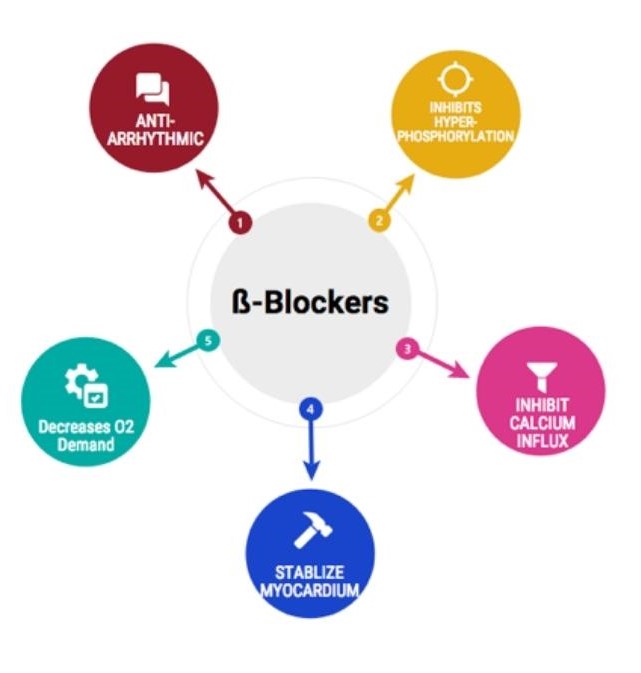
Once beta-blockers bind to the B1 and B2 receptors, they inhibit these effects. Therefore, the chronotropic (the heart rate) and inotropic (cardiac contractility) effects on the heart undergo inhibition, and the heart rate slows down as a result. The harmony of contraction of ventricular fibers gets disturbed as systole(contraction) is prolonged by delay in conduction. Beta-blockers decrease heart rate, the force of contraction, and cardiac output.
Beta-blockers also decrease blood pressure via several mechanisms, including decreased renin and reduced cardiac output. The negative chronotropic and inotropic effects lead to a decreased oxygen demand; that is how angina improves after beta-blocker usage.
These medications also prolong the atrial refractory periods and have a potent antiarrhythmic effect.
In the normal resting state effects are mild and prominent in those under sympathetic overactivity i.e., exercise, emotions.
ADVERSE EFFECTS:
On concomitant usage of drugs over a while, it has been reported to show some adverse effects like fatigue, dizziness, nausea, and constipation.
Some patients reported sexual dysfunction and erectile dysfunction.
Less commonly, bronchospasm presents in patients on beta-blockers. But Asthmatic patients are at a higher risk of exacerbation, they are contraindicated in asthmatics
Patients with Raynaud syndrome ( cold hands and feet ) are also at risk of exacerbation.
Beta-blockers can induce hypoglycemia and mask the hemodynamic signs, usually seen in a hypoglycemic patient, such as tachycardia.
Some patients report insomnia, sleep changes, and nightmares while using beta-blockers. This effect is more pronounced with beta-blockers that cross the blood-brain barrier.
All beta-blockers, especially in patients with cardiac risk factors, carry a risk of heart block.
Carvedilol may increase edema in some patients.
Sotalol blocks the potassium channels in the heart and thereby induces QT prolongation. It increases the risk of torsades de pointes which is a specific type of abnormal heart rhythm.
PHARMACOGENOMICS:
- Propranolol - CYP2D6 gene - Patients with the CYP2D6*1 allele may have lower S-propranolol plasma concentration when treated with propranolol as compared to patients with the CYP2D6*10 allele. However, contradictory findings are reported. Other genetic and clinical factors may also influence a patient‘s metabolism of propranolol.
- Metoprolol - CYP2D6 gene - CYP2D6 gene polymorphisms have been reported to interact in the metabolism of the drug.
- Carvedilol - CYP2D6 gene - CYP2D6 gene polymorphisms have been reported to interact in the metabolism of the drug.
These are some of the reported and used SNP’s used in understanding the metabolism of the drugs.
DRUG INTERACTIONS :
- Cardiac arrest can occur if beta-blockers are given along Calcium channel blockers like Digitalis and Verapamil due to additive depression of sinus nodes and A-V conduction, but propranolol can be safely used with Nifedipine.
- Propranolol has a hypoglycemic effect, when taken along with insulin severe hypoglycemia can occur. Warning signals of hypoglycemia should be looked for.
- Proton pump inhibitors like Cimetidine inhibit propranolol metabolism, dose alterations are to be done if given together.
And several other drug interactions have been reported.
BETA-BLOCKERS AND REBOUND HYPERTENSION :
Beta-blockers are drugs used in the treatment of hypertension, sudden withdrawal of beta-blockers causes rebound hypertension, worsening of angina, and sudden death in some.
It occurs due to the supersensitivity of beta receptors as a result of long-term reduction in agonist stimulation. Which on sudden withdrawal, increases beta-receptor action of vasoconstriction and causes a rise in blood pressure. Hence, compliance with beta-blockers is very important in maintaining blood pressure.
A gradual reduction in the dosage of beta-blockers should be done before weaning the patient off beta-blockers.
With recent advancements in medicine and genomics, where we can predict one‘s risk for conditions like stroke, hypertension, coronary artery disease, etc. through single nucleotide polymorphisms. Those at risk can be advised on lifestyle modifications and also adherence to treatment to prevent serious conditions and diseases from occurring.
We can also predict the efficacy, toxicity, and metabolism of drugs through pharmacogenomics, which can help in personalizing treatment best suited for an individual.
Let’s say that a person has a high risk of developing toxic effects with drug A as per his pharmacogenomics profile, then drug B which has been reported to show lesser or baseline risk for adverse effects can be used, preventing the drug-induced ailments.
This would be very much beneficial in planning better treatment plans and strategies to promote longevity, prevent diseases with modifiable risk factors, and improve the overall health of an individual.


